Reasons for Swollen Feet During Pregnancy

Swollen feet are a common companion to the miraculous journey of pregnancy, stemming from a combination of physiological changes and increased demands on the circulatory system. As the body nurtures a growing life within, blood volume surges, causing fluid retention in various tissues, including the feet. Hormonal shifts play a pivotal role, promoting relaxation of blood vessels and allowing for increased fluid accumulation. The expanding uterus exerts pressure on major blood vessels, hindering efficient circulation and contributing to swelling in the lower extremities. Prolonged standing or sitting can exacerbate this swelling, emphasizing the importance of regular movement and elevation of the feet. While edema during pregnancy is typically benign, it is essential to distinguish it from conditions like preeclampsia. If your feet become swollen during your pregnancy, it is suggested that you speak to a podiatrist who can offer you effective relief methods.
Pregnant women with swollen feet can be treated with a variety of different methods that are readily available. For more information about other cures for swollen feet during pregnancy, consult with Lance Greiff, DPM from Great Neck Podiatry. Our doctor will attend to all of your foot and ankle needs.
What Foot Problems Can Arise During Pregnancy?
One problem that can occur is overpronation, which occurs when the arch of the foot flattens and tends to roll inward. This can cause pain and discomfort in your heels while you’re walking or even just standing up, trying to support your baby.
Another problem is edema, or swelling in the extremities. This often affects the feet during pregnancy but tends to occur in the later stages.
How Can I Keep My Feet Healthy During Pregnancy?
- Wearing orthotics can provide extra support for the feet and help distribute weight evenly
- Minimize the amount of time spent walking barefoot
- Wear shoes with good arch support
- Wear shoes that allow for good circulation to the feet
- Elevate feet if you experience swelling
- Massage your feet
- Get regular, light exercise, such as walking, to promote blood circulation to the feet
If you have any questions please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Pregnancy and Foot Health
Many pregnant women complain about foot pain while they are expecting. Foot pain can primarily be caused by weight gain and hormonal changes taking place in the body. By understanding how pregnancy impacts the health of a woman's feet, a pregnant woman can take action to keep her feet as healthy and comfortable as possible.
Because a woman's weight changes during pregnancy, more pressure is brought to bear on both the legs and the feet. This weight shift can cause two major foot problems: over-pronation, also known as flat feet, as well as edema, which is swelling of the feet. Over-pronation occurs when the arch of the foot flattens, causing the foot to roll inwards when the individual is walking, and can aggravate the plantar fascia tissues located along the bottom of the feet. If these tissues become inflamed, a pregnant woman can experience pain in the heel of the foot as well as severe foot pain while walking or standing. Swelling of the feet, or edema, often occurs in the later stages of pregnancy. It is caused by slow circulation and water retention, and may turn the feet a light purple color.
To keep feet in good health and prevent over-pronation, pregnant women should avoid walking barefoot and be sure they are wearing shoes that offer good arch support. A device known as an orthotic can be added to regular footwear in order to provide additional support for the feet during pregnancy. Any expectant mother whose feet hurt should first check to see if the shoes she is wearing are old, worn out and not offering the proper support necessary for distributing the weight of her body during pregnancy.
To treat edema of the feet, a good start is to wear quality footwear which offers support and good circulation. Keep feet elevated whenever possible by using a foot stool while seated. Stay well hydrated by drinking plenty of water to prevent water retention in the feet. Any swelling that occurs in only one foot should be examined as soon as possible by a doctor.
Good foot health during pregnancy can help expectant mothers avoid foot pain that leads to other health problems. Massaging the feet and doing regular gentle exercise like walking aids foot health by contributing to good circulation. Supportive shoes are also a good investment that will support foot health during pregnancy.
Can Vitamin Deficiencies Cause Cracked Heels?

Cracked heels are a common foot problem, causing discomfort and often aesthetic concerns. While several factors contribute to this issue, vitamin deficiency is an often overlooked culprit. Specifically, vitamins A, C, and E play important roles in maintaining skin health. Vitamin A is essential for skin repair and maintenance. This type of deficiency can lead to dry, flaky skin, making it more prone to cracking. Vitamin C is known for its role in collagen production, a protein vital for skin strength and elasticity. Without enough vitamin C, skin can become fragile and susceptible to fissures. Additionally, vitamin E is a powerful antioxidant that helps protect skin from damage and maintains its moisture balance. A shortage of vitamin E can result in dry, rough skin, making the heels more likely to crack. To combat cracked heels, a balanced diet rich in these essential vitamins, along with proper foot care, is essential. Ensuring you have an adequate intake of these vitamins can go a long way in keeping your heels smooth and healthy. If you have cracked heels, it is strongly suggested that you are under the care of a podiatrist who can offer effective prevention techniques and treatment for this condition.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Lance Greiff, DPM from Great Neck Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Causes of Ankle Pain Without Injury

Ankle pain, even in the absence of apparent injury, can be a perplexing and discomforting experience. Arthritis, a common culprit, may inflame the ankle joints, causing persistent pain and stiffness. Inflammatory conditions, such as rheumatoid arthritis, can exacerbate discomfort. Likewise, Achilles tendinitis, marked by inflammation of the Achilles tendon, often induces ankle pain, particularly during movement. Structural issues such as flat feet or high arches may contribute to ankle pain by altering the distribution of weight and impacting joint alignment. Nerve compression, as seen in conditions like tarsal tunnel syndrome, can also manifest as ankle discomfort without external trauma. Additionally, overuse or repetitive strain from activities like prolonged standing or walking may strain the ankle ligaments and muscles, resulting in pain. Understanding the diverse sources of ankle pain beyond visible injuries is important for an accurate diagnosis and targeted intervention. If you have unexplained ankle pain, it is suggested that you contact a podiatrist who can determine what the reason is, and offer correct treatment methods.
Foot and ankle trauma is common among athletes and the elderly. If you have concerns that you may have experienced trauma to the foot and ankle, consult with Lance Greiff, DPM from Great Neck Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Foot and ankle trauma cover a range of injuries all over the foot; common injuries include:
- Broken bones
- Muscle strains
- Injuries to the tendons and ligaments
- Stress fractures
Symptoms
Symptoms of foot and ankle injuries vary depending on the injury, but more common ones include:
- Bruising
- Inflammation/ Swelling
- Pain
Diagnosis
To properly diagnose the exact type of injury, podiatrists will conduct a number of different tests. Some of these include sensation and visual tests, X-rays, and MRIs. Medical and family histories will also be taken into account.
Treatment
Once the injury has been diagnosed, the podiatrist can than offer the best treatment options for you. In less severe cases, rest and keeping pressure off the foot may be all that’s necessary. Orthotics, such as a specially made shoes, or immobilization devices, like splints or casts, may be deemed necessary. Finally, if the injury is severe enough, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot and Ankle Trauma
Broken Feet
A broken foot can either refer to a fracture or a straight break. The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Broken Ankles
Broken ankles are a serious injury that can lead to an inability to walk, function, and also cause a significant amount of pain. A broken ankle is a break in one of the three bones in your body that connect at the ankle joint, the tibia, the fibula, and the talus. The tibia and fibula are your two primary leg bones that connect at the knee, which sits directly upon the talus bone. This is protected by a fibrous membrane that allows for movement in our ankle joint. A broken ankle is usually caused by the foot rolling under or twisting too far, causing one of these three bones to snap.
A broken ankle is different from an ankle sprain, which occurs when the ligaments are ripped or torn but no bones have been broken. A sprain can still be very severe, causing bruising in the foot and an inability to hold your own weight, much like a broken ankle would. If you’re unable to stand, and suspect that you have a broken ankle, the first thing to do would be to get an immediate x-ray to determine the severity of the break.
A common cause of broken ankles is when the ankle is rolled over with enough pressure to break the bones. This usually happens during exercise, sports, or other physical activities. Another common cause is a fall or jump from a tall height.
One immediate treatment for pain relief is elevating the feet above your head to reduce blood flow to the injured area. You can also apply ice packs to your ankles to help reduce swelling, redness, inflammation, and pain. After these initial steps, getting a cast and staying off your feet as much as possible will aid in the recovery of the broken ankle. The less movement and stress the ankle has to endure, the more complete it will heal. A doctor can determine if surgery is needed in order to heal correctly. In these cases, an operation may be the only option to ensure the ability to walk properly again, followed by physical therapy and rehabilitation.
It is highly important to determine if surgery is needed early on, because a broken ankle can become much more severe than you realize. If not professionally treated, the broken ankle will inhibit your walking, daily functioning, and produce a large amount of pain. Treating your broken ankle early on will help prevent further damage to it.
Peripheral Neuropathy

Common peroneal nerve dysfunction, also known as common fibular nerve dysfunction, involves damage to the peroneal nerve, affecting movement and sensation in the foot and leg. This condition can occur at any age and is a type of peripheral neuropathy, specifically mononeuropathy, where a single nerve is damaged. Causes can range from knee trauma, fibula fracture, tight casts, habitual leg crossing, to pressure during sleep or surgery. It is also seen in individuals with anorexia, autoimmune conditions, diabetes, alcohol use, or inherited disorders like Charcot-Marie-Tooth disease. Symptoms include decreased sensation, numbness, tingling in the leg, foot dropping, a slapping gait, toe dragging, and muscle weakness. Diagnosis involves a physical exam, electromyography, nerve conduction tests, MRI, and nerve ultrasound. Potential complications may include reduced walking ability and permanent sensation loss or weakness in the legs or feet. If you have symptoms of peripheral neuropathy, it is suggested that you schedule an appointment with a podiatrist to discuss treatment options.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Lance Greiff, DPM from Great Neck Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Arthritis Can Cause Pain in the Feet and Ankles
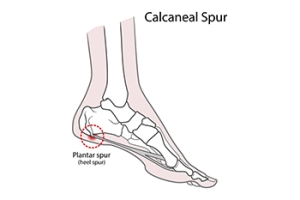
Relationship of Heel Spurs to Plantar Fasciitis

It is a common misconception that heel spurs are the primary cause of heel pain. In reality, heel spurs, which are bony projections on the heel bone, are often found by having an X-ray taken, and cause pain in only 5 percent of individuals with them. The majority of heel pain is generally due to plantar fasciitis, an inflammation of the plantar fascia tissue which stretches from the heel to the toes. While many individuals with plantar fasciitis also have heel spurs, the pain is typically from the damaged plantar fascia, not the spurs themselves. Heel spur syndrome and plantar fasciitis share similar risk factors, like athletic stress, obesity, calf tightness, high arches, and possibly osteoarthritis. Both conditions often respond to non-surgical treatments, including rest, footwear changes, and stretching. If these do not work, injections or plantar fasciotomy surgery might be recommended, though the heel spur is typically not removed during surgery. If you have heel pain, it is strongly suggested that you make an appointment with a podiatrist for a proper diagnosis and correct treatment methods.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Lance Greiff, DPM from Great Neck Podiatry. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Great Neck Bronx, NY . We offer the latest in diagnostic and treatment technology to meet your needs.