Peripheral Neuropathy

Common peroneal nerve dysfunction, also known as common fibular nerve dysfunction, involves damage to the peroneal nerve, affecting movement and sensation in the foot and leg. This condition can occur at any age and is a type of peripheral neuropathy, specifically mononeuropathy, where a single nerve is damaged. Causes can range from knee trauma, fibula fracture, tight casts, habitual leg crossing, to pressure during sleep or surgery. It is also seen in individuals with anorexia, autoimmune conditions, diabetes, alcohol use, or inherited disorders like Charcot-Marie-Tooth disease. Symptoms include decreased sensation, numbness, tingling in the leg, foot dropping, a slapping gait, toe dragging, and muscle weakness. Diagnosis involves a physical exam, electromyography, nerve conduction tests, MRI, and nerve ultrasound. Potential complications may include reduced walking ability and permanent sensation loss or weakness in the legs or feet. If you have symptoms of peripheral neuropathy, it is suggested that you schedule an appointment with a podiatrist to discuss treatment options.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Lance Greiff, DPM from Great Neck Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Arthritis Can Cause Pain in the Feet and Ankles
Relationship of Heel Spurs to Plantar Fasciitis

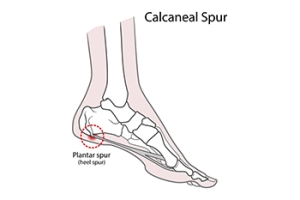
It is a common misconception that heel spurs are the primary cause of heel pain. In reality, heel spurs, which are bony projections on the heel bone, are often found by having an X-ray taken, and cause pain in only 5 percent of individuals with them. The majority of heel pain is generally due to plantar fasciitis, an inflammation of the plantar fascia tissue which stretches from the heel to the toes. While many individuals with plantar fasciitis also have heel spurs, the pain is typically from the damaged plantar fascia, not the spurs themselves. Heel spur syndrome and plantar fasciitis share similar risk factors, like athletic stress, obesity, calf tightness, high arches, and possibly osteoarthritis. Both conditions often respond to non-surgical treatments, including rest, footwear changes, and stretching. If these do not work, injections or plantar fasciotomy surgery might be recommended, though the heel spur is typically not removed during surgery. If you have heel pain, it is strongly suggested that you make an appointment with a podiatrist for a proper diagnosis and correct treatment methods.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Lance Greiff, DPM from Great Neck Podiatry. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Great Neck Bronx, NY . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Hammertoe Is a Common Foot Deformity

Hammertoe is a prevalent and often uncomfortable foot deformity that affects the toes, typically the second, third, or fourth toes. The condition gets its name from the toe's appearance, as the affected toe tends to bend or contract at the middle joint, resembling a hammer. Hammertoes can result from various causes, including wearing poorly fitting footwear that squeezes the toes and forces them into an unnatural position. High heels, in particular, are known culprits. Hammertoe can also be caused by an imbalance in the muscles, tendons, or ligaments that control the toe's movement, leading to an abnormal bend. Some individuals may have a genetic predisposition to the condition. Arthritis, injury, or nerve damage can also contribute to the development of hammertoes. The deformity can lead to discomfort, corns, calluses, or open sores due to friction with shoes. Early intervention is essential, and conservative treatments may be successful. In severe cases, surgery may be necessary to straighten the affected toe. If you have developed hammertoe, it is suggested that you visit a podiatrist who can determine its severity, followed by choosing the best course of treatment for you.
Hammertoes can be a painful condition to live with. For more information, contact Lance Greiff, DPM of Great Neck Podiatry. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the tendons, muscles, or ligaments that are responsible for holding the toes in their normal position. This condition may be caused by poor footwear, foot structure, trauma, and disease. The most common solution for hammertoe is to relieve the pain by changing your footwear and wearing orthotics. In severe cases, surgery may be required.
The shoes that are most likely to cause hammertoe are high heeled shoes or shoes that are too tight in the toe box. Tight shoes will force your toes to crowd together in a curled position. This position will likely continue when you take your shoes off. Another cause is trauma. When you stub your toe, you are increasing the chance that you will develop hammertoe.
There are risk factors that may make you more likely to develop this condition. Women are more likely to have the condition compared to men, and it is also more likely to appear in those who are older in age.
Many different foot problems can be avoided by wearing shoes that have adjustability, adequate toe room, and low heels. Furthermore, if you want to buy new shoes, you should look to purchase them at the end of the day and make sure you know your correct size. The importance of buying shoes at the end of the day is that your feet swell as the day progresses. You should also ensure that you are wearing your correct size because your shoe size may change as you grow older.
To diagnose someone with hammertoe, your podiatrist will need to conduct a thorough examination of your foot. Your doctor may even order an x-ray to evaluate the bones and joints of your feet and toes.
If you have hammertoe, your podiatrist may recommend that you wear shoes that fit you better along with inserts to place inside them. Additionally, he or she may suggest special exercises for you to perform to stretch your toes. One helpful exercise it to pick up marbles with your feet or crumple a towel with your toes.
Prior to meeting with your podiatrist, it will be helpful to make a list of all the symptoms you are experiencing. You should also make a note of medications you are taking and important personal information about your medical history.
Understanding What Arthritis in the Feet Feels Like
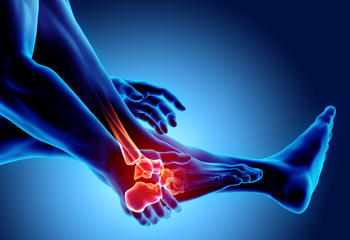
Arthritis in the feet is a condition that can bring a range of discomforts and unique sensations. It often manifests as pain and stiffness in the joints, making every step a potential challenge. Individuals with foot arthritis may experience a deep, aching pain that worsens with movement. This discomfort can be present in various areas of the foot, including the toes, the midfoot, or the ankle. One common sensation associated with foot arthritis is a feeling of stiffness or inflexibility. It can be particularly pronounced in the morning or after periods of inactivity. As arthritis progresses, swelling and warmth may accompany the pain, making the affected foot feel tender to the touch. In more advanced cases, individuals may notice a grinding or popping sensation in the affected joints, indicating the wear and tear of the cartilage. Understanding what arthritis in the feet feels like is essential for timely diagnosis and effective management. If you have any of the above symptoms which may indicate arthritis in the feet, it is suggested that you schedule an appointment with a podiatrist who can guide you toward relief methods.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Lance Greiff, DPM from Great Neck Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
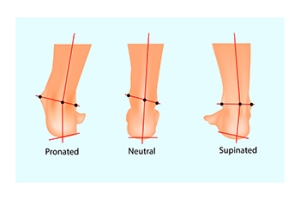
The Dangers of Excessive Supination
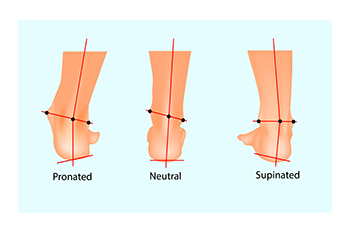
Supination, or underpronation, occurs when your body weight shifts to the outer edges of your feet during walking or running. In a normal stride, your foot should gently roll inward, or pronate, distributing your weight evenly across the ball of the foot, and pushing off using the big toe. In supination, most of the weight is on the outer edge, with push-off from the outer toes. These faulty foot mechanics can have significant implications for overall health. Excessive supination can lead to issues such as back and hip pain, knee stress, ankle injuries, and heel pain. The abnormal weight distribution also increases the risk of chronic pain and injuries, and makes you more susceptible to ankle problems and other foot conditions. Supination can result from inherited structural problems in the foot, like high arches. Weakness in the muscles of the foot, ankle, and leg can also contribute. Footwear that lacks sufficient support, body misalignment, or prior foot injuries that have damaged tendons or muscles can also be factors. To address problems caused by excessive supination, it is suggested that you make an appointment with a podiatrist who can diagnose your structural foot problems, perform a gait analysis, and provide appropriate treatment options.
If you have any concerns about your feet, contact Lance Greiff, DPM from Great Neck Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.