Causes of Ankle Pain Without Injury

Ankle pain, even in the absence of apparent injury, can be a perplexing and discomforting experience. Arthritis, a common culprit, may inflame the ankle joints, causing persistent pain and stiffness. Inflammatory conditions, such as rheumatoid arthritis, can exacerbate discomfort. Likewise, Achilles tendinitis, marked by inflammation of the Achilles tendon, often induces ankle pain, particularly during movement. Structural issues such as flat feet or high arches may contribute to ankle pain by altering the distribution of weight and impacting joint alignment. Nerve compression, as seen in conditions like tarsal tunnel syndrome, can also manifest as ankle discomfort without external trauma. Additionally, overuse or repetitive strain from activities like prolonged standing or walking may strain the ankle ligaments and muscles, resulting in pain. Understanding the diverse sources of ankle pain beyond visible injuries is important for an accurate diagnosis and targeted intervention. If you have unexplained ankle pain, it is suggested that you contact a podiatrist who can determine what the reason is, and offer correct treatment methods.
Foot and ankle trauma is common among athletes and the elderly. If you have concerns that you may have experienced trauma to the foot and ankle, consult with Lance Greiff, DPM from Great Neck Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Foot and ankle trauma cover a range of injuries all over the foot; common injuries include:
- Broken bones
- Muscle strains
- Injuries to the tendons and ligaments
- Stress fractures
Symptoms
Symptoms of foot and ankle injuries vary depending on the injury, but more common ones include:
- Bruising
- Inflammation/ Swelling
- Pain
Diagnosis
To properly diagnose the exact type of injury, podiatrists will conduct a number of different tests. Some of these include sensation and visual tests, X-rays, and MRIs. Medical and family histories will also be taken into account.
Treatment
Once the injury has been diagnosed, the podiatrist can than offer the best treatment options for you. In less severe cases, rest and keeping pressure off the foot may be all that’s necessary. Orthotics, such as a specially made shoes, or immobilization devices, like splints or casts, may be deemed necessary. Finally, if the injury is severe enough, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot and Ankle Trauma
Broken Feet
A broken foot can either refer to a fracture or a straight break. The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
Broken Ankles
Broken ankles are a serious injury that can lead to an inability to walk, function, and also cause a significant amount of pain. A broken ankle is a break in one of the three bones in your body that connect at the ankle joint, the tibia, the fibula, and the talus. The tibia and fibula are your two primary leg bones that connect at the knee, which sits directly upon the talus bone. This is protected by a fibrous membrane that allows for movement in our ankle joint. A broken ankle is usually caused by the foot rolling under or twisting too far, causing one of these three bones to snap.
A broken ankle is different from an ankle sprain, which occurs when the ligaments are ripped or torn but no bones have been broken. A sprain can still be very severe, causing bruising in the foot and an inability to hold your own weight, much like a broken ankle would. If you’re unable to stand, and suspect that you have a broken ankle, the first thing to do would be to get an immediate x-ray to determine the severity of the break.
A common cause of broken ankles is when the ankle is rolled over with enough pressure to break the bones. This usually happens during exercise, sports, or other physical activities. Another common cause is a fall or jump from a tall height.
One immediate treatment for pain relief is elevating the feet above your head to reduce blood flow to the injured area. You can also apply ice packs to your ankles to help reduce swelling, redness, inflammation, and pain. After these initial steps, getting a cast and staying off your feet as much as possible will aid in the recovery of the broken ankle. The less movement and stress the ankle has to endure, the more complete it will heal. A doctor can determine if surgery is needed in order to heal correctly. In these cases, an operation may be the only option to ensure the ability to walk properly again, followed by physical therapy and rehabilitation.
It is highly important to determine if surgery is needed early on, because a broken ankle can become much more severe than you realize. If not professionally treated, the broken ankle will inhibit your walking, daily functioning, and produce a large amount of pain. Treating your broken ankle early on will help prevent further damage to it.
Peripheral Neuropathy

Common peroneal nerve dysfunction, also known as common fibular nerve dysfunction, involves damage to the peroneal nerve, affecting movement and sensation in the foot and leg. This condition can occur at any age and is a type of peripheral neuropathy, specifically mononeuropathy, where a single nerve is damaged. Causes can range from knee trauma, fibula fracture, tight casts, habitual leg crossing, to pressure during sleep or surgery. It is also seen in individuals with anorexia, autoimmune conditions, diabetes, alcohol use, or inherited disorders like Charcot-Marie-Tooth disease. Symptoms include decreased sensation, numbness, tingling in the leg, foot dropping, a slapping gait, toe dragging, and muscle weakness. Diagnosis involves a physical exam, electromyography, nerve conduction tests, MRI, and nerve ultrasound. Potential complications may include reduced walking ability and permanent sensation loss or weakness in the legs or feet. If you have symptoms of peripheral neuropathy, it is suggested that you schedule an appointment with a podiatrist to discuss treatment options.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with Lance Greiff, DPM from Great Neck Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is a condition in which the nerves in the body become damaged from a number of different illnesses. Nerves from any part of the body, including the foot, can be damaged. There are several forms of neuropathy including peripheral neuropathy, cranial neuropathy, focal neuropathy, and autonomic neuropathy. Furthermore there is also mononeuropathy and polyneuropathy. Mononeuropathies affect one nerve while polyneuropathies affect several nerves. Causes of neuropathy include physical injury, diseases, cancers, infections, diabetes, toxic substances, and disorders. It is peripheral neuropathy that affects the feet.
The symptoms of neuropathy vary greatly and can be minor such as numbness, sensation loss, prickling, and tingling sensations. More painful symptoms include throbbing, burning, freezing, and sharp pains. The most severe symptoms can be muscle weakness/paralysis, problems with coordination, and falling.
Podiatrists rely upon a full medical history and a neurological examination to diagnose peripheral neuropathy in the foot. More tests that may be used include nerve function tests to test nerve damage, blood tests to detect diabetes or vitamin deficiencies. Imaging tests, such as CT or MRI scans, might be used to look for abnormalities, and finally nerve or skin biopsies could also be taken.
Treatment depends upon the causes of neuropathy. If the neuropathy was caused by vitamin deficiency, diabetes, infection, or toxic substances, addressing those conditions can lead to the nerve healing and sensation returning to the area. However if the nerve has died, then sensation may never come back to the area. Pain medication may be prescribed for less serious symptoms. Topical creams may also be tried to bring back sensation. Electrical nerve stimulation may be used for a period of time to stimulate nerves. Physical therapy can strengthen muscle and improve movement. Finally surgery might be necessary if pressure on the nerve is causing the neuropathy.
If you are experiencing sensation loss, numbness, tingling, or burning sensations in your feet, you may be experiencing neuropathy. Be sure to talk to a podiatrist to be diagnosed right away.
Arthritis Can Cause Pain in the Feet and Ankles
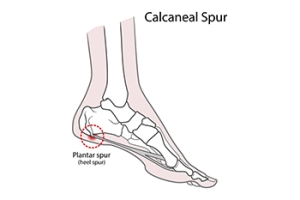
Relationship of Heel Spurs to Plantar Fasciitis

It is a common misconception that heel spurs are the primary cause of heel pain. In reality, heel spurs, which are bony projections on the heel bone, are often found by having an X-ray taken, and cause pain in only 5 percent of individuals with them. The majority of heel pain is generally due to plantar fasciitis, an inflammation of the plantar fascia tissue which stretches from the heel to the toes. While many individuals with plantar fasciitis also have heel spurs, the pain is typically from the damaged plantar fascia, not the spurs themselves. Heel spur syndrome and plantar fasciitis share similar risk factors, like athletic stress, obesity, calf tightness, high arches, and possibly osteoarthritis. Both conditions often respond to non-surgical treatments, including rest, footwear changes, and stretching. If these do not work, injections or plantar fasciotomy surgery might be recommended, though the heel spur is typically not removed during surgery. If you have heel pain, it is strongly suggested that you make an appointment with a podiatrist for a proper diagnosis and correct treatment methods.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Lance Greiff, DPM from Great Neck Podiatry. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Great Neck Bronx, NY . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Hammertoe Is a Common Foot Deformity

Hammertoe is a prevalent and often uncomfortable foot deformity that affects the toes, typically the second, third, or fourth toes. The condition gets its name from the toe's appearance, as the affected toe tends to bend or contract at the middle joint, resembling a hammer. Hammertoes can result from various causes, including wearing poorly fitting footwear that squeezes the toes and forces them into an unnatural position. High heels, in particular, are known culprits. Hammertoe can also be caused by an imbalance in the muscles, tendons, or ligaments that control the toe's movement, leading to an abnormal bend. Some individuals may have a genetic predisposition to the condition. Arthritis, injury, or nerve damage can also contribute to the development of hammertoes. The deformity can lead to discomfort, corns, calluses, or open sores due to friction with shoes. Early intervention is essential, and conservative treatments may be successful. In severe cases, surgery may be necessary to straighten the affected toe. If you have developed hammertoe, it is suggested that you visit a podiatrist who can determine its severity, followed by choosing the best course of treatment for you.
Hammertoes can be a painful condition to live with. For more information, contact Lance Greiff, DPM of Great Neck Podiatry. Our doctor will answer any of your foot- and ankle-related questions.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the muscles, tendons, or ligaments that normally hold the toe straight. It can be caused by the type of shoes you wear, your foot structure, trauma, and certain disease processes.
Symptoms
- Painful and/or difficult toe movement
- Swelling
- Joint stiffness
- Calluses/Corns
- Physical deformity
Risk Factors
- Age – The risk of hammertoe increases with age
- Sex – Women are more likely to have hammertoe compared to men
- Toe Length – You are more likely to develop hammertoe if your second toe is longer than your big toe
- Certain Diseases – Arthritis and diabetes may make you more likely to develop hammertoe
Treatment
If you have hammertoe, you should change into a more comfortable shoe that provides enough room for your toes. Exercises such as picking up marbles may strengthen and stretch your toe muscles. Nevertheless, it is important to seek assistance from a podiatrist in order to determine the severity of your hammertoe and see which treatment option will work best for you.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Hammertoe
Hammertoe is a foot deformity that occurs due to an imbalance in the tendons, muscles, or ligaments that are responsible for holding the toes in their normal position. This condition may be caused by poor footwear, foot structure, trauma, and disease. The most common solution for hammertoe is to relieve the pain by changing your footwear and wearing orthotics. In severe cases, surgery may be required.
The shoes that are most likely to cause hammertoe are high heeled shoes or shoes that are too tight in the toe box. Tight shoes will force your toes to crowd together in a curled position. This position will likely continue when you take your shoes off. Another cause is trauma. When you stub your toe, you are increasing the chance that you will develop hammertoe.
There are risk factors that may make you more likely to develop this condition. Women are more likely to have the condition compared to men, and it is also more likely to appear in those who are older in age.
Many different foot problems can be avoided by wearing shoes that have adjustability, adequate toe room, and low heels. Furthermore, if you want to buy new shoes, you should look to purchase them at the end of the day and make sure you know your correct size. The importance of buying shoes at the end of the day is that your feet swell as the day progresses. You should also ensure that you are wearing your correct size because your shoe size may change as you grow older.
To diagnose someone with hammertoe, your podiatrist will need to conduct a thorough examination of your foot. Your doctor may even order an x-ray to evaluate the bones and joints of your feet and toes.
If you have hammertoe, your podiatrist may recommend that you wear shoes that fit you better along with inserts to place inside them. Additionally, he or she may suggest special exercises for you to perform to stretch your toes. One helpful exercise it to pick up marbles with your feet or crumple a towel with your toes.
Prior to meeting with your podiatrist, it will be helpful to make a list of all the symptoms you are experiencing. You should also make a note of medications you are taking and important personal information about your medical history.
Understanding What Arthritis in the Feet Feels Like
Arthritis in the feet is a condition that can bring a range of discomforts and unique sensations. It often manifests as pain and stiffness in the joints, making every step a potential challenge. Individuals with foot arthritis may experience a deep, aching pain that worsens with movement. This discomfort can be present in various areas of the foot, including the toes, the midfoot, or the ankle. One common sensation associated with foot arthritis is a feeling of stiffness or inflexibility. It can be particularly pronounced in the morning or after periods of inactivity. As arthritis progresses, swelling and warmth may accompany the pain, making the affected foot feel tender to the touch. In more advanced cases, individuals may notice a grinding or popping sensation in the affected joints, indicating the wear and tear of the cartilage. Understanding what arthritis in the feet feels like is essential for timely diagnosis and effective management. If you have any of the above symptoms which may indicate arthritis in the feet, it is suggested that you schedule an appointment with a podiatrist who can guide you toward relief methods.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Lance Greiff, DPM from Great Neck Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Great Neck Bronx, NY . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.